Suspected/Confirmed patients should be ISOLATED & wear PPE
Treating Staff – (should not be; non-immunised, pregnant or immunocompromised)
- single-use, disposable gloves
- single-use, disposable apron (or gown if extensive splashing or spraying, or performing an aerosol generating procedure (AGP))
- FFP3 – respiratory protective equipment (RPE)
- eye/face protection (goggles or visor)
Patient
- Surgical face mask
Background
- Measles is highly infectious – (4 day prior to and after rash appears) suspected patients should be isolated within the ED
- Measles Immunisation – 1 dose 90% effective, 2 doses 95% effective
- Measles is a notifiable disease

Clinical
 Incubation –typically 10-12days but could be 7-21day
Incubation –typically 10-12days but could be 7-21day
Prodrome 3C’s – Coryza, Cough, Conjunctivitis, often symptoms peak on first day of rash
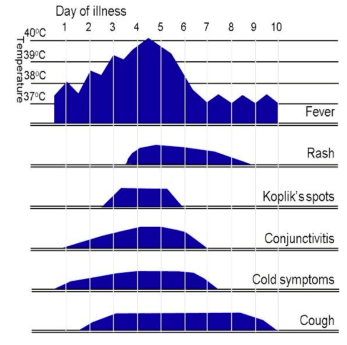
Fever – typically increases during the prodromal phase, peaks (generally >39°C) around the rash onset, as shown in Figure 1, and will gradually decrease after that.
Maculopapular rash – generally starts on the face and behind the ears. The number of lesions/spots generally increase in the first 2-3 days, and their distribution expands further to the face, trunk, and can sometimes be generalised. Lesions can become confluent, particularly on the face and the trunk. The rash is red, blotchy, maculopapular (That is non-vesicular), not itchy, and generally lasts for 3-7 days, fading gradually [6].
 Koplik spots “grain of salt on a red background” – may appear around the time of the rash, sometimes one day before, and last for 2-3 days after the rash appears. These are small spots with white or bluish- white lesions, of about 2-3mm in diameter, on an erythematous base on the buccal mucosa. These can be confused with other lesions in the mouth and therefore their suspected presence is an unreliable marker for measles.
Koplik spots “grain of salt on a red background” – may appear around the time of the rash, sometimes one day before, and last for 2-3 days after the rash appears. These are small spots with white or bluish- white lesions, of about 2-3mm in diameter, on an erythematous base on the buccal mucosa. These can be confused with other lesions in the mouth and therefore their suspected presence is an unreliable marker for measles.
Contact microbiology if:
- At Risk Groups
- Pregnant women measles can lead to an increased risk of prematurity and fetal loss, although there is no evidence that it leads to congenital defects.
- Infants under 1yr, who are more likely to develop complications and require hospitalisation
- Immunocompromised patients, esp. patients who have recently undergone bone marrow transplantation, patients with primary T-cell dysfunction, AIDS patients and patients with acute lymphoblastic leukemia (ALL)
LABORATORY DIAGNOSIS
- PCR – A viral swab (Green lid) should be used to obtain a buccal sample for PCR. (DO NOT use charcoal base swabs)
- Rub the swab against the cheeks and gums for a minimum of 20 seconds.
- Request for IgM and/or viral RNA. Ensure date of symptom onset is on request form.
- Place “Infection Risk” sticker is on sample bottle and request form and place in sample bag, then place in a second bag, ideally a purple IPC bag (if transported externally e.g. across sites must also be in a rigid container).
Hand deliver to lab vacuum tube must not be used
- Serology
- In adults and children >10 years, send a serum sample for measles IgG and IgM, this is particularly useful where measles re-infection is suspected (i.e. measles following one of more measles vaccines)
Treatment
- Supportive treatment and Isolation is effective for most
- Notify Public Health
Prognosis/Complications
- Most cases are uneventful and self limiting – and could be managed at home
- Most Frequent Complications
- Viral pneumonitis
- Otitis media
- Tracheobronchitis “measles croup”
- Rare Complication
- Encephalitis <0.1%
- Subacute Scleorsing Panencphalitis <0.01% and present years after infection
Managing Contacts
All significant contacts must be recorded on a contact tracing sheet for risk assessment, this is the responsibility of the nurse in charge of the area or clinical commander. The period of infectiousness generally starts from about 4 days before the rash and lasts up to 4 days after the onset of rash, a significant contact is defined as any person, patient or staff, who:
- Had face to face contact with index patient for any length of time. (<1m)
- Spent >15 minutes with someone with suspected measles in a closed space (triage room, ward bays, waiting room or any similar poorly ventilated area).
- For immunocompromised patients, any level of contact is considered significant.
Contact tracing forms are available on the intranet https://intranet.cht.nhs.uk/clinical-information/infection-prevention-control/organisms under Measles. One for patients and one for staff. All sections of these forms must be completed. These help to guide you through the risk assessment