There has been a resent increase in cases of Legionnaires Disease in the North West. So remember to request Urine Legionella Antigen test, if you have suspicions.
Category: Infection Control
Rabies [notifiable disease]
Recent Incident: Bat contact was not recognized (effectively touching a bat without gloves means treatment is recommended)

Rabies is an acute viral encephalomyelitis caused by members of the lyssavirus genus. The UK has been declared “Rabies-Free”. However, it is known that even in “Rabies-Free” counties the bat population posse a risk.
In the UK the only bat to carry rabies is the Daubenton’s Bat [Picture on the Left] and this is not a common bat in the UK. The UK and Ireland are Classified as “low-risk” for bat exposure. Despite our “low-risk” status in 2002 a man died from rabies caught in the UK from bat exposure.
Although rabies is rare it is fatal so we must treat appropriately, Public Health England – Green book details this.
Risk Assessment
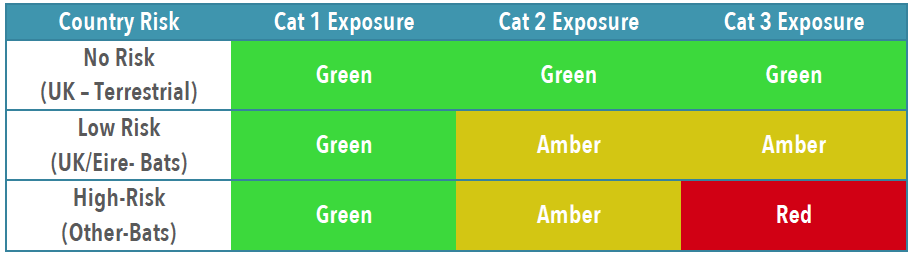
To establish patients risk and thus treatment you need to establish the Exposure Category and Country Risk [Link to Country Risk]
Exposure Category

Combined Country/Animal & Exposure Risk
Treatment
Obviously patients with wounds will need appropriate wound care and cleaning, specifics for rabies are below.
If in ANY doubt, or you feel you need advice about treatment contact: On-Call Microbiologist (who will contact PHE or Virology advice)

You will likely need to liaise with the duty pharmacist to obtain vaccine or HRIG – which may need to be sent from a different hospital. [it is probably worth trying to obtain the 1st weeks treatment if possible, to avoid treatment delays]
IN HOURS 08:30AM-5PM PLEASE CALL PHARMACY TO INFORM THEM TO EXPECT A DELIVERY OF IMMUNOGLOBULIN SO THIS CAN BE SEGREGATED FOR THE CORRECT PATIENT. PLEASE ASK TO SPEAK TO THE RESPONSIBLE PHARMACIST CRH (4218/4279) HRI (2422/7123)
Rabies and Immunoglobulin Service (RIgS), National Infection Service, Public Health England, Colindale (PHE Colindale Duty Doctor out of hours): 0208 327 6204 or 0208 200 4400
Measles
Suspected/Confirmed patients should be ISOLATED & wear PPE
Treating Staff – (should not be; non-immunised, pregnant or immunocompromised)
- single-use, disposable gloves
- single-use, disposable apron (or gown if extensive splashing or spraying, or performing an aerosol generating procedure (AGP))
- FFP3 – respiratory protective equipment (RPE)
- eye/face protection (goggles or visor)
Patient
- Surgical face mask
Background
- Measles is highly infectious – (4 day prior to and after rash appears) suspected patients should be isolated within the ED
- Measles Immunisation – 1 dose 90% effective, 2 doses 95% effective
- Measles is a notifiable disease

Meningitis – Adults
- Keep your suspicions high – early signs it may not be clear
- Sepsis Kills – give antibiotics & fluid early
- Consider Acyclovir
- Give Dexamethasone with Antibiotics – it can reduce neurological sequelae
- Consider indications for CT before LP
- Get SENIOR support early
OPAT – Cellulitis 2023
Our OPAT service can provide IV antibiotics for cellulitis for those patients that can be managed as out patients but either require IV antibiotics or have failed oral therapy.
Avian Flu – 2022
Avian flu is droplet spread and can sometimes effect humans as well as birds. Severity varies in human cases varies widely from mild to severe and deaths have been reported.
Case Definition = Clinical Criteria + Exposure Criteria
Gentamicin – Prescribing on EPR
Do NOT use this regime for:
- Pregnant women
- Children under 16 years
- Urology surgery prophylaxis patients
- ANY patient who has ascites, limb amputation, cystic fibrosis, endocarditis, major burns, Cisplatin Chemotherapy, renal transplant.
Be #urosceptical
Ditch the Dipstick – for patients >65Yrs or Catheterised!
Approx. 50% of over 65’s and most of those with catheters have asymptomatic bacteriuria. The patient will not benefit from treatment and often gives us premature closure (i.e. we blame a fictitious UTI for the patients symptoms and stop thinking). Read more
Notifiable Diseases
Registered Medical Practitioners in England and Wales have a statutory duty to notify Public Health about the following diseases. To facilitate rapid treatment and control of outbreaks. (Links to Wikipedia for illustrative purposes) Read more